BLOGS

Nonsurgical Treatment Options for Diabetic Foot Ulcers
Diabetic foot ulcers, often known as DFUs, are a common and highly complex side effect of diabetes that, if left untreated, can have catastrophic consequences. Due to the increasing prevalence of diabetes, DFUs are now considered a fundamental open prosperity concern. Efficient management and handling of DFUs are critical to preventing complications such as infection, discharge, and delayed recovery. Nonsurgical treatment choices can continuously appropriately control and mend DFUs, even if cautious interventions are occasionally significant. This article delves into the various nonsurgical options for treatment for diabetic ulcer on foot, providing a comprehensive overview for patients, caregivers, and medical professionals.
Diabetic Foot Ulcers: What Is It?
Diabetic foot ulcers are open lesions or injuries that typically develop on the foot of individuals with diabetes. They result from a combination of factors, including prolonged pressure on specific areas of the foot, poor circulation, and peripheral neuropathy. Treating these ulcers is challenging due to underlying conditions associated with diabetes, such as impaired wound healing and increased susceptibility to infection.
1. Wound Care Management
Supervising diabetic foot ulcers treatment requires genuine twisted care. This combines cleansing, debridement, and dressing to expedite healing and prevent illness.
1.1 Debris Removal and Cleaning
Cleaning the injury is vital for eliminate flotsam and jetsam, dead tissue, and microorganisms that could forestall recuperating. Debridement is crucial for advancing a sound injury bed since it eliminates dead or degraded tissue. A few debridement techniques include mechanical, enzymatic, autolytic, and meticulous. Each has benefits and drawbacks of its own.
1.2 Dressing Selection
When it comes to injury care, dressing decisions are profound. Dressings hold the wound in place, maintain moisture, and aid healing. Different dressings are available, including alginates, foam dressings, hydrogels, and hydrocolloids; each is suitable for distinct stages of wound healing and exudate levels.
1.3 Preventing infections
An essential aspect of wound care is infection management. Effective antimicrobials or cleaning agents can reduce bacterial load, and systemic antimicrobial treatments are recommended if evidence of infection extends beyond the wound. Routine observation and proactive intervention are crucial to prevent serious complications.
2. Offloading Techniques
Retouching requires reducing the burden on the ulcerated region. Offloading techniques include shifting weight and releasing pressure from the injured foot.
2.1 Total Contact Casts (TCC)
It is believed that amount to contact initiatives offer the best quality level for treating diabetic foot ulcers stages. By evenly distributing the weight over the foot, these projects lessen the strain on the ulcerated area and encourage mending. Treatment with TCCs is standard for foot ulcers and seems to accelerate healing.
2.2 Removable Cast Walkers
Another sensible offloading option is diabetic walking boots or removable cast walkers. Compared to TCCs, these gadgets provide security and ease of surveying and changing clothes. They are essential for patients who need to be seen during visits or have trouble staying in an entire cast.
2.3 Orthotic Insoles and Custom Footwear
The purpose of orthotic insoles and custom-made shoes is to reallocate and replace lost weight from high-risk areas. Custom-fitted to the individual's foot shape and ulcer location, these devices offer a practical strategy for gradual offloading and anticipating future ulcers.
3. Advanced Therapies
A few cutting-edge medications have been developed to improve diabetic foot ulcer care. These medications use bioengineered skin substitutes, negative weight wound treatment, and improvement parts.
3.1 Growth Factor Therapy
Improvement components are constantly occurring proteins that support the growth of cells and the healing of wounds. Improvement factors, such as platelet-determined improvement figures (PDGF), have demonstrated efficacy in promoting granulation tissue remodeling and inducing wound closure in healing diabetic foot ulcers.
3.2 Bioengineered Skin Substitutes
The goal of bioengineered skin substitutes is to mimic the structure and components of human skin. Products like Dermagraft and Apligraft can expedite healing and provide a platform for enhancing underutilized tissue. They are essential for treating severe, non-healing ulcers that do not respond to standard medications.
3.3 Negative Pressure Wound Therapy (NPWT)
Vacuum-aided closure (VAC) is another term for adverse weight wound treatment, which involves applying an appropriate dressing to the injury to create a controlled pull. This therapy improves circulation, draws out exudate, and reduces and decreases edema, all of which create the ideal environment for healing. By all accounts, NPWT appears to be effective in managing complicated and complex diabetic ulcer on Toe.
4. Nutritional Support
Good food plays a fundamental role in healing wounds—the body's increased need for repair and regeneration results in longer healing durations for diabetes specialist Arizona.
4.1 Protein Intake
Acceptable protein affirmations are critical for wound healing because they provide the necessary structure squares for tissue repair. In your low-fat eating routine, you should remember food sources high in protein, like lean meats, fish, eggs, dairy items, vegetables, and nuts. Protein supplements may be advised for those with more significant needs or low-income dietary habits.
Read also: Type 1 & 2 Diabetes: Taking Control Through Natural Remedies
4.2 Micronutrients
Specific minerals and nutrients are essential for wound healing. Vitamin A promotes immune function and epithelialization, while vitamin C is necessary for collagen formation. Zinc is vital for both immune response and cell division. Adjusting the diet to incorporate more whole grains, vegetables, and calorie-dense foods can help meet these micronutrient requirements.
4.3 Staying Hydrated
It is expected that proper hydration will be overlooked for both daily well-being and the healing of wounds. Drying out might impede the flow of oxygen to the injured area and the circulatory system. Encouraging patients to consume pleasant liquids, particularly water, is essential to maintain optimal hydration levels.
5. Blood Glucose Control
Managing diabetic foot ulcers requires a practical arrangement of blood glucose levels. Complete glycemic control can hinder the healing of wounds and raise the risk of contamination.
5.1 Medication Management
Patients with diabetes should closely collaborate with their healthcare providers to optimize their medication regimen. This may involve switching medications, adjusting insulin dosages or oral hypoglycemic agents, or utilizing continuous glucose monitoring systems to achieve better glycemic control.
5.2 Lifestyle Modifications
Modifications in lifestyle, such as regular exercise and eating less, are crucial for maintaining stable blood glucose levels. It is important to provide patients the freedom to engage in physical exercise, like walking, and to follow a diabetes-friendly diet that emphasizes whole grains, lean proteins, healthy fats, and minimal sugar.
5.3 Regular Monitoring
Regular blood glucose monitoring is essential for identifying hyperglycemia early and initiating appropriate action. The best ways to use glucometers and help patients understand the value of maintaining a blood glucose journal will help them monitor their progress and treatment plans.
6. Adjunctive Therapies
Several more medications can help treat diabetic foot ulcers and essential nonsurgical treatments.
6.1 Electrical Stimulation Therapy
Low-level electrical streams are used in electrical instigation therapy to promote cell growth and advance the circulatory system to the injured location. This treatment can accelerate the current veins' course of action, lessen inflammation, and promote tissue repair, enhancing the recovery plan. It is regularly utilized to recognize expected outcomes of various injury care modalities.
6.2 Ultrasound Therapy
Ultrasound therapy uses high-frequency sound waves to enhance tissue repair and reduce discomfort. This treatment can improve blood flow to the affected area, accelerate collagen production, and aid in wound healing. It is particularly beneficial for persistent, non-healing ulcers when used in conjunction with other treatments.
Read also: Potential of Infusion Therapy for Diabetes Management
The Bottom Line
Handling diabetic foot ulcers requires a multifaceted strategy that addresses the underlying causes, expedites healing, and avoids complications. Using nonsurgical treatment options, such as unloading techniques, advanced medications, back health, blood glucose management, guidance, and supplementary medications, is crucial to getting the best results. Medical professionals can essentially increase the level of personal satisfaction for people with diabetic foot ulcers and reduce the likelihood of certification complications by adopting a thorough and patient-focused strategy.
Managing diabetic foot ulcers can be challenging, but with the correct information, tools, and support, patients can achieve exceptional recovery and long-term foot health. Early intervention, adherence to treatment guidelines, and regular monitoring are crucial for effective management. By prioritizing these practices, patients can significantly improve their outcomes and maintain foot wellness.
Welcome to Gilbert Integrative Medical Center, your trusted source for comprehensive diabetes care in Arizona. Request an appointment online or by phone today.
Contact Us
Email: support@gilbertimc.com
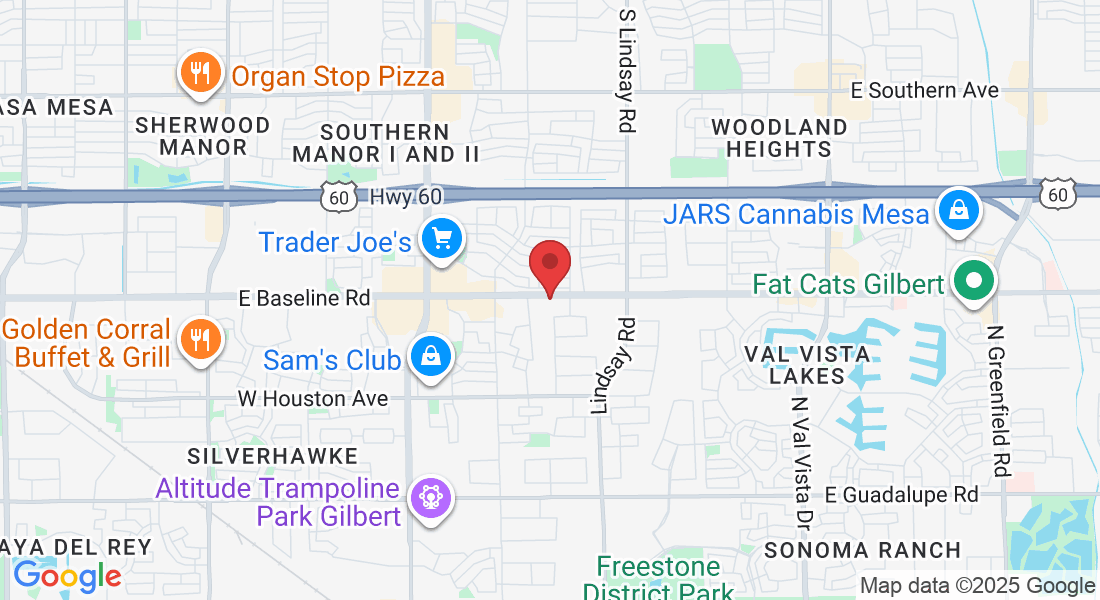
Address:
2451 E Baseline Rd #100
Gilbert, AZ 85234
Phone Number:
Stay Connected:
Visit Us
Contact Us
Email: staff@wellness1stimc.com
Address:
2451 E Baseline Rd #100
Gilbert, AZ 85234
Phone Number:
Copyright 2024 . All rights reserved